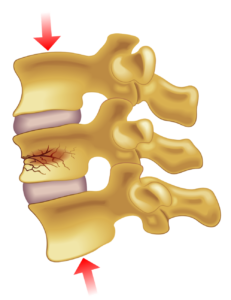
Spinal compression fractures are the result of weak bones in the spine that create small fractures within a vertebra bone of your spine. The vertebra of your spine stack on top of each other with soft discs in between to allow flexion, and this entire system is what supports your weight, protects your spinal cord, and allows your to bend and move the back. When fractures happen in your vertebra they can collapse and shorten the height of your spine. These compression fractures can also cause bone to press on the spinal cord and surrounding spinal nerves, which may cause pain and various other symptoms depending on severity.
Compression fractures generally happen in the upper back in the lower section of this portion of the spine, but they can happen in any vertebrae of the spine. They also frequently occur in the upper lumbar section, or the lower back.

Vertebral Compression Fracture
Vertebral compression fractures are called this because they are compression fractures of the vertebral body and cause the collapse of the vertebra. People who have severe osteoporosis are at much higher risk of vertebral compression fractures and may experience them while performing daily activities like lifting a light object, everyday bending or twisting of the spine, or walking about. Those who only have moderate osteoporosis might experience a compression fracture through some kind of forceful impact like a fall, lifting a heavy object, or other kind of trauma to the spine. Though patients without osteoporosis can also suffer a compression fracture during a significant impact such as a car accident, sports injury or sufficiently hard fall.
Vertebral compression fractures affect women much more often than men, but are still a major health concern for older men. The risk and occurrence increases with age, and if you’ve suffered a fracture previously the risk is much higher of a second injury occurring.
Causes of Osteoporosis and Brittle Bones
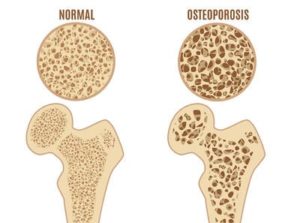
Osteoporosis is the main cause of compression fractures, so what is it? This is a bone thinning condition which creates more brittle bones that are susceptible to fracture. The risk of osteoporosis is much higher in women over the age of 50 who have gone through menopause. The body either loses too much bone, doesn’t make enough bone or a combination of both, which creates a weaker bone structure. The bones lose a great deal of density and mass, having large holes and space in the bone. Typically a bone has a tight honeycomb structure to give the bone it’s strength, but with osteoporosis the bones become more “porous” looking with the space in the honeycomb structure drastically increasing. Osteoporosis is a common condition and about half of women over 50 will experience some kind of bone breaking due to osteoporosis. The most common bones to be damaged due to osteoporosis are the hip, wrist and spine, but this can sometimes affect other bones as well.
It’s not extremely apparent that a patient has osteoporosis since a person can’t feel their bones weakening, and the first sign of it is often after a bone has broken, or the shortening of the spine due to a vertebral compression fracture. Additional risks of osteoporosis occurring aside from age and sex include low calcium intake, thyroid problems, and medical conditions like rheumatoid arthritis, cancer, kidney disease, and other diseases.
Wedge Compression Fracture
Sometimes a vertebral compression fracture is called a wedge compression fracture because when the vertebra collapses it creates a wedge like shape with the front of the bone collapsing and the back maintaining it’s height. This causes a slight hunch in the upper back and can shorten the height of a person’s spine. This is also the most common compression fracture type. When more than one vertebra experiences a fracture it’s called multiple compression fractures, and can lead to a deformity of the upper back. Another type of fractures are the crush fracture, in which the entire bone breaks instead of just the frontside of the vertebra. The other type is called the burst fracture, where there is loss of height in the front and back walls of the bone.
Compression Fracture Symptoms
One of the most prominent signs of a compression fracture you may notice at first is back pain. The problem is back pain is associated with a wide variety of spine and back related issues, so what are the other accompanying symptoms of a compression fracture? The more common indications that you may have a compression fracture include:
- The back pain comes on suddenly
- Trouble bending or twisting the spine
- Loss of height in the back
- Curved or stooped back shape
- Pain gets worse walking or standing, but improves when laying down
- Pain increases when pressure is applied to the area
- Recent trauma such as a fall, or even a minor event
Compression Fracture Treatment and Diagnosis
Diagnosing a compression fracture can often be done through physical examination and medical history, but there are a number of imaging tests which are useful in helping confirm the diagnosis, and further deduce the extent of the fracture and assist in formulating the best possible treatment plan for the patient. Imaging tests such as X-rays, CT scans, and MRI scans are all very useful for your doctor to come up with accurate diagnosis, prognosis and treatment.

Once the diagnosis is confirmed a treatment plan can begin. It’s important to treat vertebral compression fractures early, or as soon as they are detected, because if left untreated the risks of many back issues and various other health risks such as blood clots and pulmonary issues increase. Using pain medication such as NSAIDs and acetaminophen can help control pain while treatment ensues, as well as muscle relaxants and medications for nerve and bone pain can be prescribed. A back brace provides support to the back and limits the motion of the fractured vertebrae like a cast, and limiting the movement of the spine may help reduce pain. Rest for a short period of time is also helpful, with limited activity such as physical therapy while the bones heal. There are also bone strengthening medications called bisphosphonates which help to restore bone loss, as well as calcium and vitamin D supplements. If all these conservative treatments aren’t effective in restoring normal function of the spine, there are spinal surgical options that are effective at treating compression fractures.
How long to wear back brace for a compression fracture?
Back braces are a common aid to those who have suffered a compression fracture. Back supporting devices are also called orthotics or an orthosis, which is molded and conforming to your body like a cast to help stop the spine from moving. The brace will take the pressure off the vertebral body as to prevent further damage and allow healing to take place. Your doctor will guide you in how long you should wear the brace each day, and what duration the brace should be worn based on your condition. Generally, compression fractures take up to 3 months to fully heal, and a brace is worn to aid the healing process. However, wearing a brace can cause weakening of the muscles in the back since it supports the spine for you, so after using the brace for some time you will want to gradually use it less and less while strengthening the back muscles.
Surgery for Compression Fractures
Surgical operations for compression fractures are used when conservative treatment isn’t working. Your doctor may present surgery as an option if there is evidence of a serious instability of the spine that may lead to further damage to spinal nerves. There are a couple types of surgery that can be done to help assist in the healing of a compression fracture:
- Vertebroplasty – An outpatient procedure used to treat compression fractures by injecting an acrylic bone cement into the collapsed vertebra through a small needle with X-ray guidance. The cement only takes minutes to harden which stabilizes the fracture. Only local anesthetic is necessary, though IV sedation or general anesthesia are options as well.
- Kyphoplasty – Similar to a , the kyphoplasty uses a cement to stabilize the collapsed vertebra. However, small balloons are used to expand the area and increase the height of the vertebra, with the cement being injected to fill the empty space created by the balloons.
Since these procedures are minimally invasive they have low risk and complication rates, though you should go over any risks with your doctor before considering any surgery.


